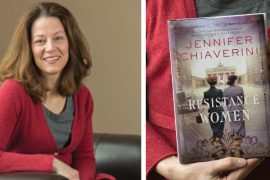
By Shelby Rowe Moyer | Photography by Rachel Coward
Here at BRAVA Magazine, we find story ideas everywhere. Sometimes they’re shared with us by readers and community members, sometimes they’re tied to current events, and sometimes they come from our own lives.
October is Breast Cancer Awareness Month, and we’ve made it our mission to cover this important topic every year. This year, we discussed life after cancer treatment (read the story here) in which we interviewed a local woman about her experience, as well as a cancer psychologist.
Narratives around breast cancer often revolve around diagnosis and treatment, but there’s an almost invisible chapter once treatment ends. The care a patient receives from their medical team tapers off, and check-ins from friends and family dissipate. Meanwhile, the person who was battling cancer is mentally, emotionally and physically catching up to everything they went through during that terrifying time.
The genesis of this year’s story came from my mother’s breast cancer journey that motivated me to pursue this angle. In 2016, my mom, Nancy Rowe — who lives in Ocean Shores, WA with her fiancé — was diagnosed with Stage III, invasive breast cancer. After undergoing treatment for about a year, she was told she is cancer-free, and she remains so to this day.
Even though my mom is cancer-free, it doesn’t mean her experience with cancer is over. She continues to live with side effects. We thought it would be insightful to give you an idea of the story-behind-the-story, so I interviewed my mom recently to hear more about her own experience with life after cancer treatment.
This has been edited for brevity and clarity.
Shelby Rowe Moyer: What cancer treatment symptoms are you going through?
Nancy Rowe: Chemobrain (memory loss). Neuropathy. Just generally not feeling good. Nothing specific that I can say; I just have off days when I don’t feel that great. People look at you and wonder what’s wrong with you. You look fine. I’m not missing my head or any limbs, but you just don’t feel good. And, if there’s an ache or a pain, my head immediately goes to: “Oh my gosh. It’s back, or it’s spread.”
SRM: Did you have any reference point for what post-treatment would look and feel like?
NR: No. Well, that’s not fair, because at my oncologist’s office — you were with me at that appointment — one of her associates went through the post-treatment timeline. They said, “This is what to expect the first year. You’re going to be having these appointments every so many months until you get to year five, and then you’ll transition to this.” You get broad brush strokes as to what it’s going to be like.
It’s hard. After treatment, it feels like a free fall. During treatment, everything is so guided and scheduled and meticulous. Family and friends are there, and they’re aware and supportive, but once you get through all that and you survived, people move on. And rightfully so. And you’re not getting all those phone calls and visits and help. You’ve survived but you’re not the same person.
Dr. Sibel Blau, [my oncologist] said it best. She said, “I may have saved you, but I really aged you.” Your body is never the same. They can’t predict how [treatment] will affect you. I never really had stomach issues before, and now I do. You’re concerned about getting your hair back, but that’s kind of the least of your worries on the other side of this. You want your pre-cancer body back and that’s never going to happen.
SRM: What was post-treatment like for you? How did it compare to going through treatment?
NR: I think the stressor for me was that I was still working full-time — just trying to navigate all these appointments, because your oncologist wants to see you, and I had a cardiologist, and [I had to see] my radiation oncologist. I tried navigating all of that while working full-time, and I did pretty well that first year. I didn’t really take any time off, but it caught up with me a year later. That’s when I ended up taking a month off.
You’re running on adrenaline for a period of time, and that definitely caught up with me. I don’t think I was prepared for that — the physical, mental and emotional exhaustion. I couldn’t get one foot in front of the other. I was living by myself for the most part. I didn’t have the stamina mentally and physically, and I still don’t. I’m probably never going to get that back.
SRM: What do you wish you had known?
NR: Definitely the physical therapy options. I had issues with scar tissue from surgery and radiation. I didn’t realize there were specialists that work with cancer patients — both pre-treatment, during and post-treatment. I had no idea. That would have been nice to know ahead of time.
SRM: Do you have any advice for others who are going through this or know someone that’s going through this?
NR: Don’t be afraid to ask for help. If you can’t be your own advocate, find someone who can be. I learned pretty quickly that you’ve got to be open and honest and let your doctors know exactly what’s going on. If people offer help, take it. And don’t be afraid to say how you’re really feeling. I think sometimes you have to remind people, that “Hey, I’m four years post-cancer. Yeah, I’m alive. I’m blessed to be a survivor, but I’m not the same.” I don’t have the same energy levels. Aging is part of it. But another big part of it is what my body went through. You don’t really know what someone else is going through. Not unless you walk in their shoes. Also, never give up. They’re making advancements all the time.